8 Steps to Ensure Accuracy in Coding for Revenue Cycle Management in the USA
Medical coding is a very important part of Revenue Cycle Management in the USA. It helps health care workers get paid correctly for the services they provide. But if coding is not done properly, insurance companies may reject the claims. Because of that, payments can get delayed, and health care workers may lose money. Also, wrong coding can cause problems in Medical Billing, making it hard for hospitals and clinics to manage their payments. So, health care workers must follow the right steps to avoid errors, speed up payments, and follow industry rules. Explore the role of medical coding in Revenue Cycle Management, steps to improve accuracy, and how tech can help. Also, how ReLi Med Solutions can support health care workers with better coding services.
Medical Coding and Its Role in Revenue Cycle Management in the USA
Medical coding is an important part of Revenue Cycle Management because it helps hospitals and clinics get the right payment for their services. But if coding is incorrect, policy companies can reject claims, which leads to financial loss. Because of that, health care workers must make sure that their coding is accurate. Here are some key points about its role:
1. Fast Claim Approval
Correct coding helps policy companies approve claims quickly. But if there are mistakes, the claim may be rejected, and payment may take longer.
2. Correct Medical Billing
Proper coding makes Medical Billing simple and ensures that hospitals and clinics get paid on time. Also, it helps avoid mistakes that can cause billing problems.
3. FHIR Compliance
By following FHIR, health care providers make sure that coding follows the latest health data-sharing rules. Because of that, medical information can be shared safely and correctly.
4. Avoid Claim Rejections
If coding is wrong, policy companies may reject claims. But correct coding helps avoid rejections, so health care providers do not lose money.
5. Organized Medical Records
Good coding helps in keeping medical records neat and easy to find. So, doctors and staff can quickly get the right patient information when needed.
6. EMR for Accuracy
EMR gives coders the right patient details. Because of that, they can choose the correct codes, and errors happen less often.
7. Smooth Billing Services
Correct coding makes it easier for billing services to process payments. Also, it helps avoid billing mistakes and delays.
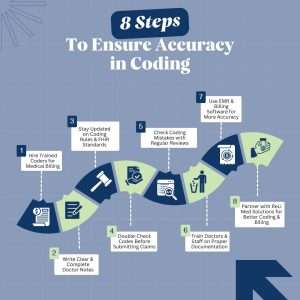
8 Steps to Ensure Accuracy in Coding
Accurate medical coding is very important for revenue cycle management because mistakes can cause claim denials and financial problems. If health care workers follow these steps, they can reduce mistakes, receive faster payments, and improve their financial system:
1. Hire Trained Coders for Medical Billing
Trained coders follow the rules correctly and make fewer mistakes. If untrained coders handle the job, they may enter wrong codes, and claims can get rejected. So, health care workers must hire skilled coders to ensure accuracy.
2. Stay Updated on Coding Rules & FHIR Standards
Medical codes change often, so coders must learn new updates in ICD-10, CPT, and HCPCS. Regular training helps them avoid mistakes and follow the latest rules. Because of that, health care workers should give coders access to ongoing training.
3. Check Coding Mistakes with Regular Reviews
Audits help find and fix mistakes before they cause claim denials. So, health care workers should conduct regular checks to ensure the medical records stay accurate and up-to-date.
4. Use EMR & Billing Software for More Accuracy
EMR and billing software help coders work faster and reduce errors. These tools also help health care workers follow Revenue Cycle Management rules and improve efficiency.
5. Write Clear & Complete Doctor Notes
Doctors must provide full and clear notes to help coders assign the correct codes. If notes are unclear, coders may enter wrong codes, which can lead to claim rejections. Because of that, doctors should always document patient details properly for medical billing.
6. Double-Check Codes Before Submitting Claims
A second coder should review the codes before submitting claims. This extra check helps catch and fix errors early, reducing the chances of claim rejections.
7. Train Doctors & Staff on Proper Documentation
Doctors and staff must write complete and detailed notes to help coders do their job correctly. Training on FHIR rules, accurate documentation, and proper coding helps reduce mistakes and improve claim approvals.
8. Partner with ReLi Med Solutions for Better Coding & Billing
ReLi Med Solutions provides expert billing services and coding support to help health care workers reduce errors, get faster claim approvals, and improve their revenue cycle.
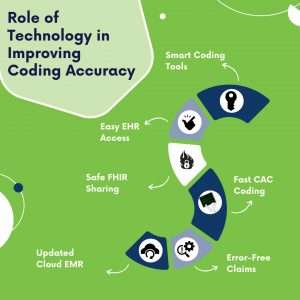
Role of Technology in Improving Coding Accuracy
errorTech has made medical coding easier and more accurate. Because of that, coders can now work faster and make less errors. Here are some ways tech helps improve coding accuracy:
1. Smart Coding Tools
AI-based tools suggest correct codes, so human mistakes decrease. But if coders rely only on manual coding, errors can still happen.
2. Easy EHR Access
EHR helps coders access correct patient details, so coding becomes more accurate. But if patient records are incomplete, mistakes in coding can still occur.
3. Safe FHIR Sharing
FHIR standards allow health care workers to share coding and billing information securely. Because of that, patient data stays safe, but if providers do not follow these standards, errors in data exchange can happen.
4. Fast CAC Coding
CAC helps coders find the correct codes faster, so manual work is reduced. But if coders do not verify the suggested codes, mistakes can still occur.
5. Error-Free Claims
This software checks for mistakes in claims before submission, so denials can be avoided. But if claims are submitted without review, policy companies may still reject them.
6. Updated Cloud EMR
Cloud-based EMR ensures coders always have the latest patient details, because of that, coding becomes more accurate, But if internet access is poor, data updates may be delayed.
FAQs
1. Why is accurate medical coding important in Revenue Cycle Management?
Correct medical coding helps health care workers get paid on time, avoid denials, and follow industry rules. Also, it makes Medical Billing smooth and problem-free.
2. What are the most common coding challenges in Billing Services?
Some common issues are frequent coding changes, missing documentation, and claim denials. But ReLi Med Solutions helps solve these problems with expert coding support.
3. How does FHIR help improve medical coding accuracy?
FHIR improves data exchange and medical coding accuracy, making sure billing is done correctly.
4. What steps should health care providers take to improve coding accuracy?
Health care workers should hire trained coders, use modern tech like EMR, conduct audits, and stay updated with coding changes.
5. How does ReLi Med Solutions help in coding and Medical Billing?
ReLi Med Solutions offers expert medical coding, billing services, and compliance support to help reduce mistakes, avoid claim denials, and improve the revenue cycle.
Conclusion
Accurate medical coding is vital for Revenue Cycle Management because it ensures health care workers get paid correctly, avoid claim denials, and follow industry regulations. But if coding mistakes happen, it can cause financial losses and delays in payments. Because of that, health care workers must follow clear steps, use advanced tech like EMR and FHIR, and work with expert coders.
ReLi Med Solutions helps with medical billing and coding to make work easier for healthcare workers. We help reduce mistakes, get payments faster, and increase earnings. If you need a trusted team for billing and coding, ReLi Med Solutions is here for you!