Optimizing Revenue Cycle Management: Metrics for QPP Success
Revenue Cycle Management helps health care workers collect payments for the services they provide. It makes sure they receive their payments on time and without problems. But in the QPP, providers also need to follow strict rules and give better patient care. The QPP, started by CMS, gives rewards to providers who improve patient care and lower costs. Because of that, tracking important numbers in RCM helps workers get better payments and avoid penalties. So, workers must watch and improve these numbers to succeed in QPP.
Why Is Revenue Cycle Management Important for QPP?
Revenue Cycle Management is important because it helps providers handle money and provide good patient care. If workers do not handle the billing process properly, they may face claim denials, late payments, and money problems. Because of that, many workers find it hard to meet QPP goals. A strong revenue cycle makes sure that Medical Billing is correct and that claims have accurate Medical Records. This helps providers receive payments quickly and follow QPP rules. But if they do not manage RCM well, they may lose money and struggle financially. Because of that, checking RCM numbers is important for success.
FAQ: What happens if RCM is not optimized?
If RCM is not working well, workers may face more claim denials, slow payments, and financial loss. This can lead to less money and QPP penalties.
The Key Metrics for RCM in QPP
To do well in QPP, workers must track vital numbers in RCM. These numbers show if their process is working well or if they are losing money. But if providers do not check these numbers, they may face claim issues and compliance problems. Here are the key numbers for Revenue Cycle Management in QPP:
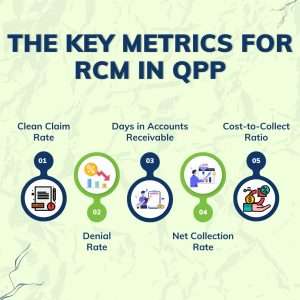
- Clean Claim Rate (CCR) – This number shows how many claims are sent without mistakes. A high CCR means fewer errors and faster payments. But a low CCR means some errors need fixing.
- Denial Rate – A high denial rate means many claims are rejected due to mistakes, missing details, or insurance issues. Because of that, providers must improve claim accuracy.
- Days in Accounts Receivable (A/R Days) – This number tells how long providers wait to get paid after sending claims. Lower A/R Days means faster payments and better cash flow.
- Net Collection Rate (NCR) – This shows how much of the total money a provider collects. A high NCR is important for financial stability.
- Patient Payment Collection Rate – More patients pay their bills directly, so tracking this number is important for steady income.
- Cost-to-Collect Ratio – This number shows how much a provider spends to collect money. A lower cost-to-collect ratio means more profit and better management.
FAQ: Which metric is most important for QPP success?
All numbers are important, but the NCR and CCR are the most important because they help workers collect more money.
ReLi Med Solutions: Simplifying Denial Management for You
Claim denials are a big problem in Revenue Cycle Management. When claims are denied often, providers lose money and spend extra time fixing mistakes. Because of that, handling denials the right way is very important for providers in QPP. ReLi Med Solutions helps providers stop denials by using smart technology, AI tools, and expert claim checks. Our advanced Billing Services help providers:
- Fix denial reasons
- Automate claim processing
- AI error check
- Appeal denied claims
- Follow QPP rules
Because of that, providers can spend less time on claim issues and focus more on patient care.
FAQ: How can providers reduce claim denials?
Providers can reduce claim denials by using automated billing services, checking patient insurance before treatment, improving coding accuracy, and working with experts like ReLi Med Solutions.
How Can Health care Providers Streamline RCM?
To make Revenue Cycle Management better, providers must find ways to work faster and avoid mistakes. But many workers struggle with slow payments, claim errors, and compliance issues. Because of that, they need to use modern tools to make their work easier. Here’s how they can do it:

- Automate Billing and Claims Processing – Using FHIR-powered automation tools helps reduce mistakes, send claims faster, and improve cash flow.
- Improve Documentation and Coding – If Medical Records are not correct, claims will be denied. So, making sure coding and documentation are accurate is very important.
- Make Patient Payments Easier – More patients pay their bills directly, so offering digital payments and flexible payment options helps workers collect money faster.
- Check Important RCM Numbers Regularly – Watching EMR-integrated RCM data helps workers find problems early and improve performance.
- Train Staff on Best Practices – Well-trained staff make less mistakes and improve claim acceptance rates.
- Work with RCM Experts – Outsourcing Billing Services to experts like ReLi Med Solutions helps workers save time, reduce costs, and collect more revenue.
FAQ: How does outsourcing RCM benefit health care workers?
Outsourcing RCM helps workers save money, avoid claim mistakes, collect payments faster, and focus more on patient care.
Conclusion
Improving Revenue Cycle Management is very important for QPP’s success. However many workers face problems because of slow billing, frequent denials, and rule changes. Because of that, tracking RCM numbers, using FHIR-based automation, and improving Medical Billing accuracy are needed. ReLi Med Solutions offers EMR-integrated RCM solutions that help providers simplify billing, reduce errors, and collect more revenue. So, by using expert solutions, health care workers can get faster payments, follow QPP rules, and succeed financially. For a better RCM experience, partner with ReLi Med Solutions today!

